The plantar fascia is a sheet of very tough material running the length of the bottom of your foot. Basically a long and flat but thick sheet of connective tissue, it attaches your heel to each of your toes. Tissues that connect bones to other bones are called ligaments, so this may also be referred to as the plantar fascia ligament.
Like other connective tissue, it is constructed primarily of a protein called collagen, in this case type I collagen. Other elements of the plantar fascia include: elastin; fibroblasts, which secrete collagen; glycosaminoglycans or GAGs, which are carbohydrates that aid in resilience; water, nerves and blood vessels.
About Plantar Fasciitis
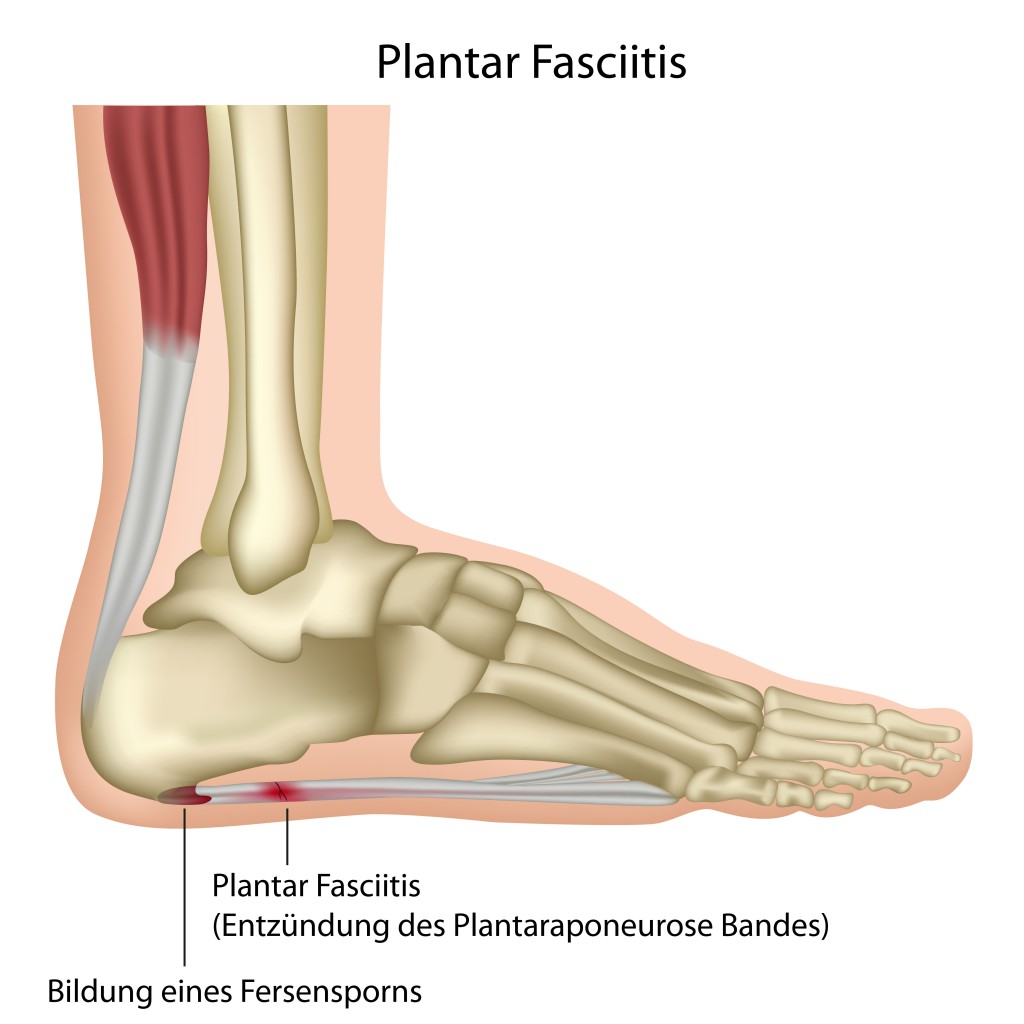
The condition called plantar fasciitis occurs when small tears or ruptures occur in the plantar fascia, causing pain especially on the bottom of the heel. The plantar fascia can also be termed the plantar aponeurosis. When the condition goes beyond inflammation and the damage becomes long-lasting, it is sometimes called plantar fasciosis. A more serious but much less common injury is plantar fascia rupture, which is a serious tear to the entire fascia rather than just micro injuries.
Something else that can damage the plantar fascia are heel spurs. These are sharp pieces of bone formed where the plantar fascia has been pulling away from where it is attached to the heel. Bony tissue is laid down at the points of separation. These can then dig into the surrounding softer tissues.
Plantar Fasciitis? Get Remedies Fast!
Symptoms
The pain from plantar fasciitis usually develops gradually and in one foot rather than both. It is felt right in the middle of the bottom of the heel where the plantar fascia has its base of attachment to the heel bone (calcaneus). Pain upon awakening is typical, with eventual lessening with activity. Often standing for a long time or abruptly arising from a seated position can worsen the pain.
Causes
The plantar fascia does more than just attach the heel bone to the toe bones. It also supports the other bones of the foot and has a biomechanical function. It can expand and contract with striding, acting as a springboard to help impel motion and helping to absorb the shock of impact with each footfall. It tensions the bottom of the foot between the heel and the toes.
It is the structure of collagen itself that enables much of this biomechanical function. The collagen is laid down in an ordered way and the strands of collagen I are arranged in a braided or rope-like manner which allows for strength and elasticity. If conditions arise which place undue stress on the plantar fascia, collagen strands can break and begin to unravel.
This results in small tears or ruptures within the plantar fascia. Fibroblasts produce new collagen to repair the damage, but it is collagen III which is not as strong or flexible as collagen I. Eventually the collagen III is replaced by collagen I, but as is typical with connective tissue, healing is slow to occur.
It used to be thought that the pain of plantar fasciitis was caused by the presence of heel spurs, since these were frequently found during diagnostic imaging. However, it has been found that people can have heel spurs without the painful symptoms, which calls this into question. If usual treatments for treating plantar fasciitis don’t bring relief, pain from bone spurs present should be investigated.
Risk Factors
Conditions which can cause tears or ruptures to occur in the plantar fascia are:
- Wearing ill-fitting or worn-out shoes.
- Being overweight.
- Having abnormalities in foot arch structure such as very high arches or low arches.
- Having an abnormal gait, especially where the feet roll inward while walking (pronation, or having flat feet).
- Exercise that stresses the heels of the feet, such as running and some types of dancing.
- Needing to stand or walk on hard surfaces for long periods of time, such as in nursing, teaching, waitressing, military personnel.
- Being over 40.
- Being female.
- Having arthritis, which can cause inflammation to tendons and ligaments.
- Having diabetes.
- Being pregnant.
Prevention Tips
Wear shoes that fit your feet and provide good arch support. Take care to replace athletic shoes before the cushioning wears out. If you run, shoes are good for about 500 miles. Avoid shoes with high heels, since these place stress on the heel and Achilles tendon, which in turn affects the plantar fascia. The Achilles tendon attaches the base of the heel to the calf muscles.
Devices which cushion and support the heel. Routine use of arch supports, orthotic devices and cushioning insoles can help prevent plantar fascia injury.
Body weight can be a factor as well so it is important to maintain a healthy body weight.
Pregnancy
With the added weight gain during pregnancy and the presence of hormones which cause softening and relaxing of connective tissue, stress is added to the plantar fascia. Care should be taken during this time to not stress out the ligament.
Sudden Changes in Exercise Routines
Before making changes to more rigorous exercises or activities such as in running longer distances, adding extra hours of practice to field sports, or escalating to more demanding routines, consideration should be given to the possibility of injuring the plantar fascia.
Stretching exercises before being active loosens the ligament and helps prevent damage, as does a gradual increase in intensity and duration of activities rather than a sudden onset. As a person ages and tendons and ligaments become more inflexible in general, care should also be taken to stretch before activity.
Correcting Inborn Gait Problems
Working with a podiatrist and/or an orthotic specialist to analyze gait irregularities and then to produce devices to correct them can lessen the likelihood of plantar fascia injury over time.

Sometimes, and especially for athletes, plantar fascia taping is recommended. Taping has to be carefully done using a special athletic tape and with the feet dry and clean. It is usually applied before activity that might stress the plantar fascia or at the beginning of a day to give the feet support in general. Tape should not be left continuously in place. It is often used in combination with orthotic supports.
Test & Diagnosis Considerations
The diagnostic heel pain which is worst upon getting out of bed is caused by the tightening of the plantar fascia during sleep. When activity is begun for the day, the ligament doesn’t move well and pain is the result. As movement warms the plantar fascia, pain often decreases. The pain is variously described as stabbing, tearing, or burning.
A physician will often press on the midheel area where the ligament joins with the heel bone to affirm the source of the pain. The foot is examined to check for swellings, tender areas and inflammation. X-rays or MRIs may be taken to rule out bone stress fractures or pinched nerves.
Pain in other areas of the foot such as the ball of the foot should not be confused with plantar fasciitis. Pain in the ball of the foot is usually associated with metatarsalgia, which is inflammation of the tissues which accompany the bones of the arch of the foot (metatarsals). Pain along the back of heel up toward the calf muscle is usually associated with Achilles tendon problems.
Treatment Options
It is important to begin treatments as soon as possible after symptoms are noted to prevent serious lasting damage to the plantar fascia. Symptoms can usually be alleviated by conservative non-surgical methods, but it can take a lengthy period of time to reverse the damage.
One of the possible consequences of not seeking prompt treatment is developing gait changes that can affect other parts of the body while attempting to favor the injured foot. Ankle, knee, hip and back problems can follow untreated plantar fasciitis.
Reducing Inflammation
Immediate icing of the painful area is helpful to reduce pain and swelling. Use something that can conform to body contours such refreezable gel packs or ice bags. Apply the ice for 20 to 30 minutes until numbness sets in; then remove for 20-30 minutes before reapplying. A combination of applying cold while stretching the plantar fascia is of benefit. Freeze water in paper cups or use a can of frozen juice. Roll one of these about under the affected foot, massaging and flexing the bottom of the foot while numbing with coldness.
Taking non-steroidal anti-inflammatory medications such as ibuprofen, aspirin, and naproxen help relieve symptoms and lessen pain. They do not affect a cure, but they usually allow a person to be more comfortable.
Stretching & Flexibility
Increasing the flexibility of the plantar fascia can help too. There are a series of foot stretches and exercises that can be performed as well as calf exercises. One exercise is to sit down, extend your leg in front of you with the knee bent and grasp the toes in one hand. Gently pull them back toward the top of the foot until you feel a pull in the arch area. This lengthens and stretches the ligament.
A towel stretch accomplishes much the same thing. Loop a rolled towel under the ball of your foot and grasp the ends of the towel in your hands. Gently pull the towel toward your body, keeping the knee straight. Hold for 15-30 seconds and repeat three or four times.
The towel curl involves sitting down, putting a towel on the floor under the foot and using the toes to gather the towel in folds, push the folds behind the foot. Then work in reverse, using the toes to push the towel forward ahead of the foot. Alternatively, you can also use your toes to “walk” your foot forward across a carpeted surface and then back toward you again. A related exercise is placing some marbles and a cup on the floor. Seated, try picking the marbles up with your toes and placing the marbles in the cup.
Additional Stretching
A simple plantar fascia/calf stretch uses stairs which have a banister or railing. Stand on one stair with the toes and ball of your feet on the tread, allowing the heels to suspend over the lower stair. Hold on to the railing or banister while doing this. Then relax your calf muscles and allow the heels to droop downward. You should feel a pull all along the bottom of your foot, through the back of your leg and to the knee. After about 30 seconds, tighten the calf muscle slightly to raise the heels again. Repeat this several times.
Another stretch is for the calf and Achilles tendon. Facing a wall, brace your hands against it, arms extended at about chest height. Step back with the damaged foot and place the foot flat on the floor. Step forward with the other foot and bend it gradually so you lean toward the wall. When you feel the stretch in your calf down toward your heel, hold for 15 to 30 seconds, then relax. Repeat this several times.
Working the Arch of the Foot
To exercise the area in the arch of the foot, sit down and put a tennis ball or rolling pin on the floor and roll it around using the area in the arch of the foot. If you can balance well, you can try doing this exercise while standing.
All exercises can be repeated several times a day for best results in strengthening the fascia and making it more flexible.
Massage is sometimes helpful. Often people undergo physical therapy to aid in recovery. A physical therapist can work with each individual to provide exercises that work for his or her set of particular circumstances. Acupuncture has also been used to treat persistent pain.
Losing Weight
Weight loss can often alleviate symptoms. Use of orthothic supports which fit inside the shoe can help cushion the heel, distribute weight better and encourage proper gait while the foot is healing. Both custom-made ones for your individual foot and off-the-shelf models work. Favor your feet by not going barefoot, even when you get up for brief periods at night. Slip on a pair of shoes which will provide arch support even for going short distances.
Resting the Foot
Another way of removing the stress, especially when severe pain is present, is to rest the foot, giving it a chance to recover from too much running, jumping, walking, dancing, or whatever behavior brought on the injury. For less severe pain, minimizing the activity for a while until pain abates is advisable. Also consider switching high-impact activities such as jogging and running for low-impact activities such as swimming or riding a stationary or regular bicycle for a while.
Taping of plantar fascia is sometimes done to help alleviate pain, although usually it is considered as primarily a preventative measure (which see).
A device known as a night splint can help lessen the pain upon awakening. The padded night splint fits along the bottom of your lower leg and the bottom of your foot, with straps around your leg and foot holding it in place. This support keeps the plantar fascia stretched while you sleep or rest.
Corticosteroid Use
If these conservative treatments do not work, injections of corticosteriods directly into the painful area may be considered. Steroids act to decrease inflammation and thus reduce pain. Injections do not always solve the problem and may worsen it by further weakening the connective tissue. Another method of providing corticosteriods to the injured area is by putting them on the skin surface and then using an electric stimulus to aid in absorption through the skin. This is called iontophoresis and is not a painful procedure.
Extracorporeal Shock Wave Therapy (ESWT)
Shock waves (sound waves) are used to bombard the injured area to stimulate it and hopefully hasten repair and recovery of the connective tissue. This is not a widely used treatment and it is still being assessed. It can cause numbness, tingling, swelling or pain over the area in which it has been used.
Surgery
The treatment of last resort is surgery. If the tissue has been so damaged that repair is unlikely, surgery to disconnect the ligament from the heel bone can be performed. Usually this is done mostly to lessen chronic severe pain when nothing else has worked. Understandably this procedure weakens the foot arch because the tension between toes and heel that the plantar fascia provides is no longer there. Side effects of the surgery can be infection, nerve injury, rupture of the plantar fascia and also no relief of pain.
After surgery support in the form of a brace or cast is needed for a varying length of time for proper healing of the tissue, with several weeks usually being needed before weight can be applied to the heel again. The usual recovery time to normal foot use is about three months.
Endoscopic surgery may also be used for a less invasive procedure. This is where small incisions are made to allow the passage of tools and a lighted camera. This procedure allows location and removal of the damaged part of the plantar fascia with less injury to surrounding tissue.
Coblation Surgery
A newer surgical technique than traditional surgery that has been used for treating plantar fasciitis is coblation surgery. The name is derived from “controlled ablation.” The technique is also called the Topaz procedure. It uses radiofrequency energy combined with a saline solution to remove tissue gently and with minimal destruction to adjacent structures.
If a heel spur seems to be causing pain by pressing into tender tissues near the bottom of the heel, steriod injections can be used here as well followed by surgery to remove the spur if injections do not relieve the pain.
Additional Resources
About.Com Treatment Options
Mayo Clinic, Plantar Faciitis Information
American Academy of Podiatric Sports Medicine

2 Comments
thank you for such nice way to explain but the question is the following:
What is the side effects on the Topaz Fasciiti procedure? since it is a new thing., pls
I was told I can have it done. I have seened how it is done, but I don’t nor I can read the side effect, I’m sure it have because everything have it good and bad side.
Thank you kindly
I have plantar fasciitis. The stretching helped but I work on my feet .
I ended up using a magnetic ankle bracelet. It has really helped. Occasionally I think it is much better and take the anklet off. Within 5 days the pain gets much worse.