Troublesome dental problems can create a mouthful of pain and discomfort for anyone dealing with a toothache. One of the biggest difficulty dental patients have regarding their dental health is how to treat and cure toothaches. Dental pain, regardless of its origin, can be so disruptive to everyday life, that millions of people each year are unable to cope effectively when the mouth pain occurs.
Toothache discomfort may range from a mild ache to excruciating throbbing pain. Whether the sufferer is experiencing pain great or small, the search for remedies to stop dental pain takes many individuals straight to their computers with the hopes of seeking out some sort of relief from the toothache.
Causes Of Tooth Discomfort
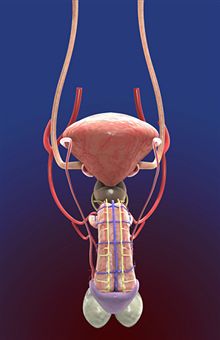
In relation to tooth discomfort, causes may range from excessive tooth decay or cavities, abscesses, broken or damaged teeth, sinus infections, and gum disease. Tooth decay is one of the most prevalent causes of illness throughout the world, especially in locations that do not promote preventative dental hygiene. Lack of brushing, flossing, and poor nutrition are also suspect in creating an environment ripe for potential dental problems.
With tooth decay, the rotten portion of the tooth tends to progress into the pulp and root of the tooth, causing pain.
If a decaying tooth is left untreated by a dental professional, the resulting damage may ultimately lead to infection and possibly the loss of the tooth. Pain and discomfort in and around the affected tooth can be quite severe.
When teeth have an excess of plaque and tartar, there is a greater risk of tooth decay and dental pain due to the increase in of digestive acids that tend to further aggravate toothache pain.
Toothache Symptoms
Quite often a toothache may appear to arise with little or no warning. However, the majority of tooth pain can be traced back to small clues that progressively worsened over time. Taking special notice to the visual condition of the tooth may give the individual an indication of why the toothache has presented itself. Important things to take notice of when experiencing a toothache:
- Broken or chipped teeth
- Pits or dark spots on tooth surface
- Small holes or crevices
- Red or swollen gum tissue
- Puss-filled bump around the base of the tooth
- Other important warning signs to look for when a toothache begins to take hold are:
- A bad taste in the mouth
- Bleeding gums
- Bad breath
- Tooth sensitivity
- Pain when chewing
- Discomfort when brushing or flossing
- Facial swelling or puffiness
- Risk Factors And Toothaches
Common risk factors and health choices that may adversely affect dental health and wellness are eating disorders such as anorexia and/or bulimia, dry mouth, poor oral hygiene habits, lack of flossing, heartburn (high levels of stomach acid may erode tooth enamel), smoking, chewing tobacco, and underlying health problems such as medications and cancer treatments. As individuals age, teeth naturally will weaken and become more susceptible to decay and sensitivity. Continuation of proper oral hygiene can help extend the health and life of teeth in older individuals.
Toothache Complications
While most people can overlook minor aches and pains associated with intermittent toothaches, ignoring serious signs of dental distress may lead to severe oral infections and tooth loss. It is essential to overall health for anyone suffering from a toothache to take immediate steps to discover the underlying cause of the tooth pain in order to avoid dangerous complications down the road.
The real threat of serious infection from toothaches must not be underestimated. Abscesses and infection can lead to sinus and blood infections which may be potentially life threatening. It is imperative to seek out medical assistance when there is the presence of infection.
Home Remedies For Toothaches
In the event that visiting the dentist for treatment must be put off briefly, finding a home remedies that can lessen toothache pain in the interim can help bring the tooth discomfort to a tolerable level. Popular and proven remedies made from natural ingredients found in most homes that may improve the pain level of a toothache are effective enough to take a closer look at.
Garlic and rock salt placed on the affected tooth, or a garlic clove positioned directly on the painful site can alleviate discomfort. Consuming raw onion, usually one per day, can improve the overall health of the teeth. Lime is well-known remedy for toothaches and oral health. The vitamin C found in lime improves tooth health. Another common home remedy for toothaches is vinegar and bayberry. The mixture of the two natural ingredients has been known to relieve mouth pain when applied to the teeth and gums.
Clove Oil
One of the most identifiable natural toothache remedies that has been in use for thousands of years is clove oil. The antiseptic properties found in cloves acts as a numbing agent when applied to the teeth and gums. Clove oil is very strong, so a little goes a long way.
Butternut Bark
In the Native American culture, the use of butternut bark for the alleviation of tooth pain has been used for many years. Another natural cure for toothache pain is asafoetida, which when applied directly to the cavity-filled tooth, will relieve even the most gnawing discomfort.
Gum Massaging
Gum massaging is an old tried-and-true natural remedy for oral pain. By gently manipulating the gums, increased blood flow occurs and effectively allows more oxygen to the affected area in order to generate healing. The use of calendula petals for toothache pain has been in use in native communities to treat dental disorders. Another effective method of treating toothaches is yarrow root. Yarrow is known for stopping a toothache that is in the beginning throws of irritation.
A largely overlooked herbal remedy that can be used as a mouthwash and antiseptic is slippery elm powder. The powder is dissolved in water and is a safe alternative to standard mouthwashes. Tarragon leaves are also an excellent choice in natural toothache prevention. Tarragon is commonly utilized as an herbal anesthetic when applied to the affected tooth.
Eastern Herbal Remedies
Eastern ayurvedic cures and remedies for toothaches employ similar herbal and mineral applications for eliminating the dental discomfort. Babool tree bark is an excellent ayurvedic herbal remedy that helps to arrest the bleeding and pain of an injured or infected tooth. The use of marjoram, which has a mint-like aroma may also be used in the natural curing of a toothache. The use of East Indian rosebay root is also an effective means of pain relief as well.
Western Herbal Toothache Remedies
There are several western home remedies available for the treatment of toothache pain. Cayenne is a wonderfully versatile natural remedy for ending the discomfort of dental pain. When used in small amounts, cayenne provides a natural local anesthetic to the painful area. A very effective natural cure for toothaches is the fig.
Figs have natural pain-relieving compounds. When heated, the fig can be placed directly on the tooth to provide immediate relief of painful abscesses and irritated gums. The use of cider vinegar has antiseptic properties that assist the natural bacteria-killing elements that are found naturally in saliva. Used as a mouthwash, cider vinegar promotes healing and germ-ridding agents.
Applied topically as a poultice, fennel helps to alleviate inflammation that so commonly aggravates the nerves of the teeth, creating pain. Sage and myrrh both provide an essential numbing effect when applied as a tincture to an irritated tooth. The antiseptic properties of both of these herbs will ease the pain of a toothache seconds after its application.
Safety And Precautions Of Herbal Toothache Cures
Most herbal remedies are completely safe and effective to use as a cure for toothaches.However, a misconception that many toothache pain sufferers fail to remember when using alternative natural toothache remedies is assuming that because it is a natural element, it must be safe to use. Caution must be maintained when ingesting or absorbing any herbal or natural remedy into the body. Natural does not always mean safe. Proper research and precautions to avoid possible toxicity and side effects must be done before attempting to use any natural toothache remedy.
Emergency Pain Relief For Nighttime Flareups
A toothache always seems to surface at the least convenient of times. The middle of the night is the most frequent time of day for mouth pain to erupt. One reason for tooth discomfort to occur at night is the position of the head when sleeping. Being in a horizontal lying position causes blood flow to be more centered around the head and mouth area. This increases the likelihood of a sensitive tooth to flare up. When late night dental pain interrupts sleep, some of the quickest methods of relieving the discomfort in order to rest throughout the night can be found in the kitchen and bathroom cupboards.

The application of an ice pack may lessen the intensity of the toothache. Alternating twenty minutes on with twenty minutes off for maximum effect. If the cold happens to worsen the discomfort, applying a warm washcloth to the cheeks may be used instead. Heat and cold both have pain relieving properties. Some people react better to one or the other.
Salt and Pepper Shakers
A strange, yet rather effective method of curbing a midnight toothache can be found in your salt and pepper shakers. Mixing the two flavor enhancers together and applying the mixture to the affected tooth can bring immediate pain relief. The use of turmeric powder in conjunction with mustard oil work well together as an antiseptic for dental pain. By applying a mixture of the two directly to the teeth, a numbing of the tooth will occur.
Using a Potato
An old remedy to stop toothache pain in its tracks can be found in a sack of potatoes. Cut a small wedge out of a raw potato and place the wedge on the affected tooth for approximately fifteen minutes. This should halt the discomfort and allow for a more restful night.
Vanilla Extract
Vanilla extract has been used for years as a home remedy for emergency toothache relief. Apply a few drops of the extract to the affected area. The toothache pain will vanish instantly. This method can be repeated as often as painful flareups occur.
Dietary And Traditional Toothache Remedies And Prevention
While the use of herbal remedies are excellent alternatives to conventional treatment options for toothaches, there are a number of traditional remedies that work very well at controlling and relieving the pain and discomfort of dental problems that can be used alternately or in conjunction with each other. Tylenol, Ibuprofen, and aspirin work well to stave off a moderately painful toothache. Rinsing the mouth with salt water can decrease mouth irritation as well.
In the unfortunate event of an excruciating toothache, the employment of any of the effective natural treatments can lessen the discomfort until a dental professional can be seen. Proper oral hygiene is always the best preventative defense against oral pain.