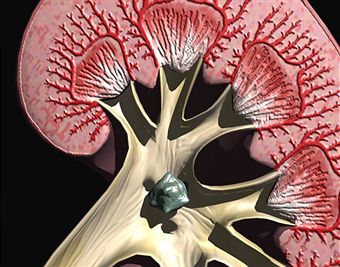
The skin is the body’s largest organ. Its functions are to protect the body, keep the body at a good temperature, and allow for the sense of touch. It is the only organ that is always exposed to the external environment. There is over 20 square feet of skin on an average human adult. The skin is made of three layers. The innermost layer is made of subcutaneous fat. This layer helps the body to stay warm. The middle layer is called the dermis. The dermis contains nerve endings, oil and sweat glands, and blood vessels. The upper layer is the epidermis. This layer is made up of mostly dead skin cells.
Any time the skin is irritated, it can become itchy. Itching is a common feeling that all people and animals get at some point in their lives. Around 20 per cent of adults experience some kind of itching on a regular basis. It can be a very discouraging and uncomfortable feeling. It is known in the medical field as pruritus.
It leads to a desire or reflex to scratch the area that is itching. Itching is a defense mechanisms which tells the spinal cord and then the brain when something is touching the nerve endings of the dermis layer of the skin. Scratching is the immediate response to the stimulus. Scratching has one goal and that is to remove whatever is bothering the skin. Itching brings on a feeling similar to that of pain, except that instead of the withdrawal reflex that pain leads to, itching leads to a scratch reflex. Itch receptors are also more sensitive than pain receptors.
Causes of Itching
There are over 1000 things that can make a person itch. For the most part, these things include anything that can touch and irritate the skin and certain diseases.
An itch can be caused by something physical or neurological. An itch can come on by skin irritation or as a symptom of another disease. Just thinking about itching can make a person want to scratch themselves. Itching can come on without any symptom at all when the skin is irritated. Itching can also be associated with dry skin, bumps, spots, blisters, or redness.
On a human, there are many small insects that can be the cause itching, whether by the presence of the insect or by its bite or sting. These include:
- Head lice
- Pubic lice
- Body louse
- Mosquito or chigger bites.
- Spider bits
- Parasitic infections
Other things that cause itching include:
- Urticaria, commonly known as hives, which is a common allergic reaction
- Fungal infections
- Certain skin conditions, such as dermatitis, psoriasis, scabies, and tinea infections. Tinea infections are commonly called ring worm, jock itch, or athlete’s foot.
- Hodgkin’s disease
- Xerosis, commonly called dry skin. This is more common in the winter time or after frequent hot baths.
- Scab healing or scar growth
- Development of moles, pimples, or ingrown hairs
- Dandruff
- Chicken pox
- Psychiatric diseases
- Certain medications
- Menopause
- Malignant or internal cancer
- Sunburns
- Dry air
- Pregnancy
- Withdrawal from certain drugs
- Chronic stress
- Some internal diseases such as liver disease, kidney failure, celiac disease, iron deficiency anemia, certain types of cancer, diabetes, or thyroid problems. In these cases, the itch usually includes the entire body.
Prevention of Itching
- If your skin is sensitive, take extra precaution when washing. Take baths instead of showers.
- Use bath oils to keep the skin moisturized.
- Use mild soaps. Supper fatted or oil based soaps are less likely to cause dryness, but should not be used all the time.
- Use moisturizer on your hands often.
- Use sunscreen when outside.
- After you get out of a bath or shower, immediately put on moisturizer.
- Use mosquito repellant.
- Drink lots of water.
- Don’t wear wool or acrylic fabrics. Cotton and silk clothing are good for itches.
- Use unscented and mild laundry detergent.
- Don’t scratch. While scratching can solve some of the less serious itches, it can also cause problems.
For the most part, avoid scratching. Long term scratching can lead to a condition called neurodermatitis. Neurodermatitis is characterized by thick, leathery skin. Scratching can also cause bacterial infections and permanent changes in skin color or even scaring.
Treatment of itching
Since itching is such a common problem, and is usually not serious, there are many remedies that can be done at home to soothe the itch. Some of these remedies are:
– Baking Soda. Baking soda can be used many different ways to relieve itches. One cup of baking soda can be added to a bath to soothe all over itches or itches that are hard to reach. A baking soda paste can also be made out of one part water and three parts baking soda. This paste is applied directly to the skin, but shouldn’t be used if the skin is broken.
- Oatmeal. One or two cups of ground oatmeal in a warm bath tub can soothe itches.
- Evaporated Milk. Add one can to a bath and let it soothe away the itch.
- Apple cider vinegar. One tablespoon in a bath can help an itch.
- Ice can often relieve the itchy area. If ice is not readily available, cold water can help.
- If it’s the hands or feet that are itching, and the reason is dryness, apply a layer of petroleum jelly and wear gloves or socks.
- Cut your nails short to avoid irritating the skin if scratching is a problem.
- If itching is caused by dry skin, a simple moisturizing lotion may be the solution.
Treating itches using herb
- Peppermint or yellow dock in a bath tub is supposed to help itches
- Burdock root oil applied to the skin will stop itching and heal rashes
- Fresh chickweed – Soak two large handfuls in water until it softens. Allow it to cool then apply onto the itching area.
- Cloves and Juniper berries – American Indians were known for using these two things to stop an itch. The berries have anti-inflammatory properties and the cloves numb nerve endings. To make this concoction, melt three ounces of unsalted butter. In a different pan, melt about two tablespoons of beeswax.
- Basil – Basil also contains a nerve numbing agent. To use on itches, place a half ounce of dried basil leaves in one pint of boiling water. Cover it and allow it to cool. Use a cloth to spread the tea onto the itch.
- Mint – mint contains substances that are both anti-inflammatory and anesthetics. Place one ounce of mint leaves in a pint of boiling water. Cover and wait until it cools. Strain the tea and use a cloth to spread the tea onto the affected area.
- Thyme -Thyme also has anesthetic and anti-inflammatory properties. Make a thyme tea using one half ounce of dried thyme in a one pint jar of boiling water. Just like the mint and basil tea, cover it and allow cooling. Strain the tea and use a cloth to spread onto the affected area. In China, this mixture will often contain an ounce of dandelion root as well.
Over the counter and store bought remedies for itching
Most over the counter medications for itching fall into two categories. They are either oral antihistamines or corticosteroid creams. Here is a list of some of the popular over the counter solutions.
- Aloe Vera Gel – Aloe vera gel is made from the aloe vera plant. When a leaf of an aloe vera plant is cut or crushed, a transparent fluid comes out. This fluid has soothing properties. It is commonly used for burns, but it also helps to relieve itching feelings. It is available for about five dollars a bottle.
- Ivarest – Ivarest temporarily relieves itching. It, like Benadryl, also blocks histamines. It can cause mild skin irritation.
- Calamine Lotion – Calamine lotion works well for itching that is associated with poison ivy, chicken pox, insect bites, and sun burns. It can occasionally irritate the skin or cause a rash. It can be bought for as little as $2 a bottle.
- Aveeno anti-itch concentrated lotion or cream – This lotion or cream brings quick relief to itches caused by minor skin irritations, insect bites, and chicken pox. There are no known side effects of the lotion. It can be bought for around $5 for an ounce of cream or $5 for 4 ounces of lotion.
Benadryl
There are many Benadryl products that can stop itching. Benadryl produces an anti itch cream that can be applied right onto the itch. It should not be used for chicken pox, measles, or on a large area of the body. Some people experience skin irritation when using the Benadryl cream. If an allergy or hives is what caused the itching, an oral Benadryl product can work to stop the itch.
Benadryl is an antihistamine. Histamines are what the body produces during an allergic reaction. Histamines cause swelling and sometimes itching. Benadryl blocks the histamines. Oral Benadryl has many side effects. Some of them include: tiredness, dizziness, coordination problems, heartburn, and thickening of bronchial secretions. All Benadryl products are available in most grocery or drug stores for under $15.
Doctors and Itching
If itching doesn’t improve in about two weeks, it is time to see a doctor. It is also good to seek medical attention if the itching is so severe that it distracts you from day-to-day activities. Unexplained itching or itches that include the entire body, or if the itch has other symptoms with it are also reasons to see a doctor.
When you see a doctor, the doctor will ask specific questions to determine the cause of the itch. The doctor may also perform certain tests if he or she thinks the cause of the itching is an internal problem.
If the doctor finds an underlying cause for the itching, he or she will treat that cause. When the cause is treating, the itching will go away. There are other ways that doctors may suggest treating itching. They include:
- Over the counter medications
- Light therapy – This is also known as phototherapy. During this procedure, the skin is exposed to specific wavelengths of ultraviolet light. Multiple sessions may be needed to get itching under control, and each session can be very expensive.
- Wet dressings – This is a process where medicated creams are put on the itchy area and then covered with a damp material made of cotton. The cotton is usually soaked in water before being applied.