Hemorrhoids
Hemorrhoids, also known as piles, are blood vessels and masses of supporting fibrous tissue inside the anus and anal canal.
The anal canal is medically described as being the area from the anus, extending inward approximately four inches, to the base of the rectum. It is widely believed that hemorrhoids are an abnormal condition of the body, but hemorrhoids are a normal anatomical feature in everyone.
When people talk about hemorrhoids as a medical condition, what they mean to say is inflamed hemorrhoids. Statistically, enlarged or inflamed hemorrhoids occur in 1 out of every 25 people.
Distribution is equal among men and women. While hemorrhoids can cause problems with people of any age, they are most prevalent in people from 45 – 65 years old. For people aged 50 and over, the incident rate rises to 50%.
Hemorrhoids are more prevalent in North America and Europe than anywhere else in the world, and there are some countries where they are virtually unknown. Several theories exist as to why this is, the two most prominent being diet and the use of sit-down commodes.
Hemorrhoids? Get Remedies Fast!
Types and Symptoms of Hemorrhoids
Hemorrhoids are differentiated into two types: external and internal. Each type has different symptoms and treatment. Because the nerves on the inside of the anal canal are visceral nerves, pain is rarely accompanied by internal hemorrhoids. Visceral nerves are sensitive only to pressure and not pain. The outside of the anus contains somatic nerves like other areas of skin that are extremely pain sensitive. The symptoms of hemorrhoids can range from mild discomfort or itching to severe pain and bleeding.
Internal Hemorrhoids
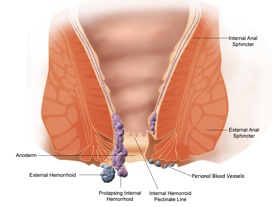
When internal hemorrhoids become inflamed, they create a large bulge in the anal canal. Sometimes the internal hemorrhoid can pull the lining of the rectum free from its anchoring so that it hangs down and can be seen on the outside of the anus. This is specifically known as a prolapsed internal hemorrhoid.
Internal hemorrhoids are subject to each stool that passes through the anal canal. Hard stools or hard matter in stool can further inflame the hemorrhoids. In some cases, the internal hemorrhoids can cause bleeding and enlarge so much that they affect the somatic nerves, causing excruciating pain.
Additionally, the prolapsed rectum continues to excrete mucus as it normally does inside the body. This mucus combines with fecal matter and when exposed to the skin of the anus it causes extreme itching. Although the prolapsed rectum usually returns inside the body on its own, but if not, it can be pushed back in. However, if it is pushed back in, it usually falls out again when passing the next stool.
In rare cases, an internal hemorrhoid cannot be pushed back inside and the blood supply to it is pinched off. This is known as an incarcerated hemorrhoid. An incarcerated hemorrhoid that is not getting any blood has a good chance of contracting gangrene.
Doctors classify internal hemorrhoids into one of four degrees, based on their severity
- First-degree hemorrhoids – These are the least severe hemorrhoids. They do not prolapse, but they can bleed.
- Second-degree hemorrhoids – These hemorrhoids prolapse, but they retract themselves without having to be pushed. They may bleed or not.
- Third-degree hemorrhoids – These hemorrhoids prolapse but do not retract on their own. They must be pushed back in and are usually accompanied by bleeding.
- Fourth-degree hemorrhoids – These are the most severe hemorrhoids. They cause a prolapse that cannot be pushed back in. Fourth-degree hemorrhoids may cause thrombosis or other loss of blood flow to the hemorrhoid.
External Hemorrhoids
External hemorrhoids, while they can be painful, are usually not as severe as internal hemorrhoids. They can be felt on the body as a bulge on the outside part of the anus. Usually, they do not interfere with the regular workings of the anus in the passing of stools, so there the stool rarely causes further inflammation.
External hemorrhoids, however, are very susceptible to thrombosis. If the hemorrhoid causes thrombosis it will turn into a hard, painful lump that usually must be treated by a medical professional. Even if the hemorrhoid heals spontaneously, it will often leave a skin tag on the anus. If the skin tag is large enough, it can continue to irritate the anus and pose difficulty in regular cleaning.
Causes of Hemorrhoids
Although no specific causes of hemorrhoids have been identified with certainty, the major cause is thought to be excessive straining during bowel movements. Other conditions may exacerbate hemorrhoids, such as cirrhosis of the liver, pregnancy, and chronic constipation or diarrhea. Sitting for long periods on the toilet also seems to have a connection with increased incidents of hemorrhoids, as does anal intercourse.
The mechanics of hemorrhoids are also not 100 percent certain, but doctors know that the arteries that are responsible for supplying blood to the rectum create a large network in the anal canal. These arteries feed the hemorrhoids and the connecting tissue. This is why when they bleed, the blood is bright red. The blood is infused with fresh oxygen from the lungs. Bleeding can be severe because the hemorrhoids have access to so many arteries.
External and internal hemorrhoids are differentiated by the dentate line, where the outside anus converts from skin to internal lining. The hemorrhoids are made up of one or more arterial blood vessels and tissues, called cushions, in three separate positions: anterior, posterior, and one lateral. Pressure during bowel movements or from other sources weakens the cushions supporting the blood vessel until they are no longer able to sufficiently hold the vessel into place, so they bulge outward and into the anal canal or the skin of the anus. When inflammation occurs in one part of the hemorrhoid, it quickly spreads to the others.
Risk Factors Associated with Hemorrhoids
Although no exact cause has been determined, several factors are associated with an increased risk in developing hemorrhoids or exacerbating already inflamed hemorrhoids
- Chronic constipation or diarrhea – Both of these conditions lead to straining during bowel movements and increased pressure in the rectum and anal canal.
- Being overweight or obese – Obesity causes extra pressure to be placed on hemorrhoids by fat deposits.
- Genetics – People with a family history of hemorrhoids are more likely to have problems with them themselves.
- Age – Older people generally have more problems with hemorrhoids than younger people.
- Pregnancy – All stages of pregnancy, including labor and delivery, put large amounts of increased pressure and strain on the entire body. Hemorrhoids are one of many areas affected, especially during the last two trimesters when the volume of blood rapidly increases.
- Liver disease – Some liver conditions cause blood to flow irregularly and this can cause inflamed hemorrhoids.
- Heart disease – Heart disease also causes an irregular flow of blood that increases risk.
- Prolonged sitting – People who sit for great lengths of time, especially on a toilet, have a higher risk for developing inflamed hemorrhoids.
- Heavy lifting – Lifting heavy objects causes pressure to build in the abdomen and anal area that can cause hemorrhoids. This is especially true for people who hold their breath as they lift.
Prevention Tips
Many instances of hemorrhoids can be avoided by following a few guidelines relating to a healthy diet and lifestyle
- Eat foods high in fiber. Whole grains, raw fruits and vegetables, and beans are excellent sources.
- Avoid foods that can cause constipation. Dairy products, such as milk, cheese, and ice cream can create constipation. It is also suggested to limit quantities of bleached grains and red meat.
- Drink sufficient amounts of water. 8 – 10 glasses of water per day is recommended.
- Avoid beverages leading to dehydration. Beverages that cause dehydration are those that contain caffeine or alcohol.
- Use natural stool softener whenever constipated. High fiber stool softeners made of bran or psyllium husks can help reduce pressure on the bowels. Never take stimulant laxatives. These only irritate hemorrhoids further.
- Exercise regularly. Moderate daily exercise helps keep the body in shape and promotes smooth digestion.
- Don’t hold in bowel movements. Go to the bathroom as soon as the urge strikes.
- Do not strain during a bowel movement. Try to let the stool be released smoothly and naturally.
- Do not sit on the toilet for extended periods. Do your business and move to a regular chair to read.
- Avoid any type of sitting for long periods. Take breaks to stretch your legs and relax your body.
- Avoid heavy lifting whenever possible.
Diagnosing Hemorrhoids
The first sign of hemorrhoids usually comes from a self-diagnosis. External hemorrhoids can be felt with the hands and are usually noticed while wiping. Bloody stool or drops of blood on bathroom tissue can also signal hemorrhoid inflammation. It is also possible to feel a prolapsed rectum exiting the anus. If left too long, a person will feel the pain associated with hemorrhoids, thrombosis, or gangrene. While discomfort of the anus and anal itching frequently occur, they are usually caused by a factor other than hemorrhoids.
Physicians usually have a good idea if a person is suffering from hemorrhoids simply from a medical history and basic questioning. Hemorrhoids are simple to diagnose, so the physician’s primary concern is to rule out other, more severe causes. This will, at the least, require a digital rectal exam and, possibly, an anoscopy, in which the doctor will visually inspect the anus and anal canal with the help of a device consisting of a hollow tube and light source. These tests are usually enough, as hemorrhoids can readily be felt by a gloved finger or seen through the anoscopy.
Tests
These tests can also help to uncover other ailments such as anal fissures or even prostate cancer. In some cases, a doctor may use what is called indirect anoscopy, which is a test that uses mirror to watch the anus while the patient is seated on a toilet or toilet-like seat. This test can help a doctor to determine the exact nature of any prolapsed tissue. Sometimes the tissue can be the hemorrhoid, and other times, it is a polyp or the rectum.
To eliminate other causes of the symptoms, a patient may be required to undergo a colonoscopy or a flexible sigmoidoscopy. A colonoscopy is a procedure where the entire colon can be inspected by the doctor, while with a sigmoidoscopy, only the rectum and anal canal are viewed. Another test that could be performed is a barium enema. This is an x-ray procedure that allows the doctor to view the colon, rectum, and anus.
Hemorrhoid Treatment
Several treatments exist in varying degrees from change of diet to surgery. Usually the most non-invasive forms of treatment are tried first, and then, if unsuccessful, treatment is scaled up. Sometimes several treatments can be used in conjunction.
General Treatment
General treatment includes lifestyle changes. A change in diet that includes more fiber will soften stool and reduce strain on the hemorrhoids. Sometimes, this is all that need be done. Following all the precautions and prevention tips may reduce hemorrhoid flare-ups to non-existence. 30 grams of fiber per day is recommended, along with plenty of water.
Over-the-counter Medication
Several different over-the-counter medications are available without a prescription, although the advice of a doctor is always beneficial. Most of these medications are in the form of creams and suppositories. They may act to relieve pain and itching, but it has never been proven that they do anything to actually cure or treat the hemorrhoids. These creams, ointments, gels, and suppositories are applied with a finger or with a special device called a pile pipe.
Here are the available over-the-counter medications for hemorrhoids
- Analgesics – These are pain relievers that may also relieve itching. Analgesics include camphor, juniper tar, and menthol.
- Antiseptics – Antiseptics are used to kill bacteria and other harmful organisms that may infect a hemorrhoid. These include benzalkonium chloride, benzethonium chloride, boric acid, hydrastis, cetylpyridinium chloride, phenol, and resorcinol.
- Astringents – An astringent promotes dryness of the skin, which can relieve itching and burning sensations. These include calamine, witch hazel, and zinc oxide.
- Corticosteroids – This type of steroid reduces inflammation and relieves itching, but long-term use can cause irreversible skin damage.
- Local Anasthetics – Anesthetics help to relieve pain and itching for a short time by temporarily deadening the nerve endings. Local anesthetics are known to cause allergic reactions. They include benzocaine, benzyl alcohol, dibucaine, dyclonine, lidocaine, pramoxine, and tetracaine.
- Protectants – These form a barrier over the hemorrhoid, protecting it from outside irritation. Protectants include aluminum hydroxide, cocoa butter, cod liver oil, glycerin, kaolin, lanolin, mineral oil, petroleum jelly, starch, and zinc oxide.
- Vasoconstrictors – Vasoconstrictors reduce the size of blood vessels. This can help to relieve pain and itching. These include ephedrine sulfate, epinephrine, and phenylephrine.
Noninvasive Treatments for Hemorrhoids
Noninvasive treatments by a doctor are usually attempted before surgery is deemed necessary, except in cases of emergency involving thrombosis, gangrene, or serious infection. These treatments rely on scarring the hemorrhoid cushions, causing the swelling to go down and leading to self-reattachment.
- Cryotherapy – This uses extreme cold to scar the tissue and reduce inflammation. It is more difficult than other treatments and may cause pain after it is completed.
- Heat coagulation – This treatment uses heat to scar the tissue. The heat can be produced either through infrared light, electricity, or another means. This treatment frequently produces moderate pain.
- Rubber band ligation – With this treatment, a rubber band is wound tightly at the base of the hemorrhoid, causing it to form an ulcer that is soon replaced with a scar. Recurrence frequently occurs with ligation one or more years later. Ligation has also been known to create infection.
- Sclerotherapy – This treatment involves injecting either phenol or quinine urea into the hemorrhoid to induce scarring. Pain may occur the following day.
Surgical Treatments for Hemorrhoids
Estimates are that less than 10% of hemorrhoid patients require surgery. Surgery is usually reserved for the most severe hemorrhoids or in emergencies.
Here are the common surgical treatments
- Dilation – Physical dilation of the sphincter can relieve pressure in the area and reduce the symptoms of hemorrhoids. Unfortunately, this type of treatment may permanently damage the sphincter and cause lifelong incontinence.
- Doppler ligation – In this procedure, the surgeon locates the main artery supplying blood to the hemorrhoid. It is tied off, and the hemorrhoid shrinks.
- Hemorrhoidectomy – This is the surgical removal of the hemorrhoids. It may require stitching and later removal. Severe pain after the surgery is very common and may require strong narcotic medications. Several complications may also occur, including urinary retention, hemorrhaging, infection, and narrowing of the anus.
- Sphincterotomy – In this treatment a cut is made in the sphincter to reduce pressure in the anal canal. Incontinence may occur afterward.
- Stapled hemorrhoidectomy – This new treatment is one of the most popular today if surgery is required. In this treatment a suture is used to pull the hemorrhoid cushions back into place. At the same time, a staple is used to trap part of the hemorrhoid in the stapler and bring together the cut tissue. The subsequent scar tissue that forms, keeps the hemorrhoids in place. External hemorrhoids may also be reduced through this surgery. It is fast (30 minutes) and much less painful than traditional surgery.
Home Remedies for Hemorrhoids
Home remedies for hemorrhoids mostly involve lifestyle changes and cleanliness. Witch hazel is commonly used to clean hemorrhoids naturally and help reduce pain and itching.
Warm showers help to relieve pressure. This is recommended several times daily, if necessary. Soaps should not be used as they cause irritants that can further inflame hemorrhoids.
A sitz bath is common home remedy for hemorrhoids. This small tub fits over a regular toilet and is used to easily soak hemorrhoids in warm water. Application of a cold compress to the anus can relieve swelling and reduce pain and itching. The use of moist towelettes or wet naps instead of dry paper can help prevent irritation of hemorrhoids.

2 Comments
Is it true that one or more grades of hemorrhoids may lead to a secondary condition that leads to vision problem?
Can you also tell me where can I go online to find all the secondary possible condition of hemorrhoids or prolapse?
Thanks,
B. Al
Thanks for this usefull article.If you wish to get rid fo hemorrhoids here are some tips : make warm sitz baths, sitting in a warm tub for 20 minutes, two or three times a day may be helpful.Stay away form spicy food may also prevent anal itching.