Alternative Names
Genital Warts is the common name given to the flat, raised or cauliflower shaped growths found in genital areas on a body and transmitted through skin-to-skin or sexual contact. They can be flesh colored, white or gray and can be raised or flat. Genital Warts arises from a sexually transmitted virus known as the human papilloma virus or HPV, of which there are more than 100 known types.
HPV is not curable and most carriers do not know they have the disease because they never exhibit symptoms. Genital Warts and HPV are the most common type of sexually transmitted disease with an estimated 80% of the adult population having contracted or carrying the disease at any given time. Infection rates for genital warts are very high and over half the people who come into contact with genital warts the first time will acquire it.
Basic Information
It has been discovered that almost 75% to 85% of sexually active adults will have contracted some form of HPV in their lifetime, regardless of whether or not they exhibit any symptoms. Genital warts are a symptom of an HPV infection. It is estimated that around 30 to 40 of the 100 known types of HPV are sexually transmitted but not all of these can lead to genital warts. The types that lead to genital warts are typically labeled as the low risk virus. That is, they do not cause abnormal cell changes that can develop into cancer.

The warts are not painful and can appear on the genital areas as well as the anus and thighs. Treatment can be done by freezing, laser treatment, electrical treatment, surgery and topical treatments; however treatment does not ensure that the warts will not return. Genital warts are not a life threatening condition, but can give rise to certain types of cancer if they are accompanied by another infection of high risk HPV.
The potential to give rise to cancer is the major area of concern when contracting HPV. The types of cancer known to be caused in part by HPV include cervical, penile and anal cancer. It is the high risk strains of the HPV virus that can cause cancer, while the low risk strains primarily cause genital warts. Thus, genital warts are not often a sign nor are they a symptom of something more serious.
Symptoms
The symptoms of a genital warts viral infection include the skin surface symptoms of flat, raised or cauliflower shaped bumps on the skin. The bumps can be white, gray or flesh colored and are not often associated with pain. Genital warts can cause discomfort during sex as they can be rubbed, pulled or stretched causing pain or bleeding. If this is occurring, seek treatment to help alleviate these symptoms and wait until treatment is complete before engaging in sexual activity.
Because of the many types of HPV, genital warts are not always visible and are often known to go away on their own. The body’s natural defenses can rid itself of a number of the types of HPV, though it is known that the person is still a carrier of the virus. Unless the person is tested further, through blood tests, once the symptom of genital warts disappears, the person may feel they are cured.
Viruses are not curable and a carrier will usually transmit that virus to other sexual partners. Tests have not been developed to detect HPV in men and the only test for women is designed to screen for high risk types of HPV that cause cervical cancer.
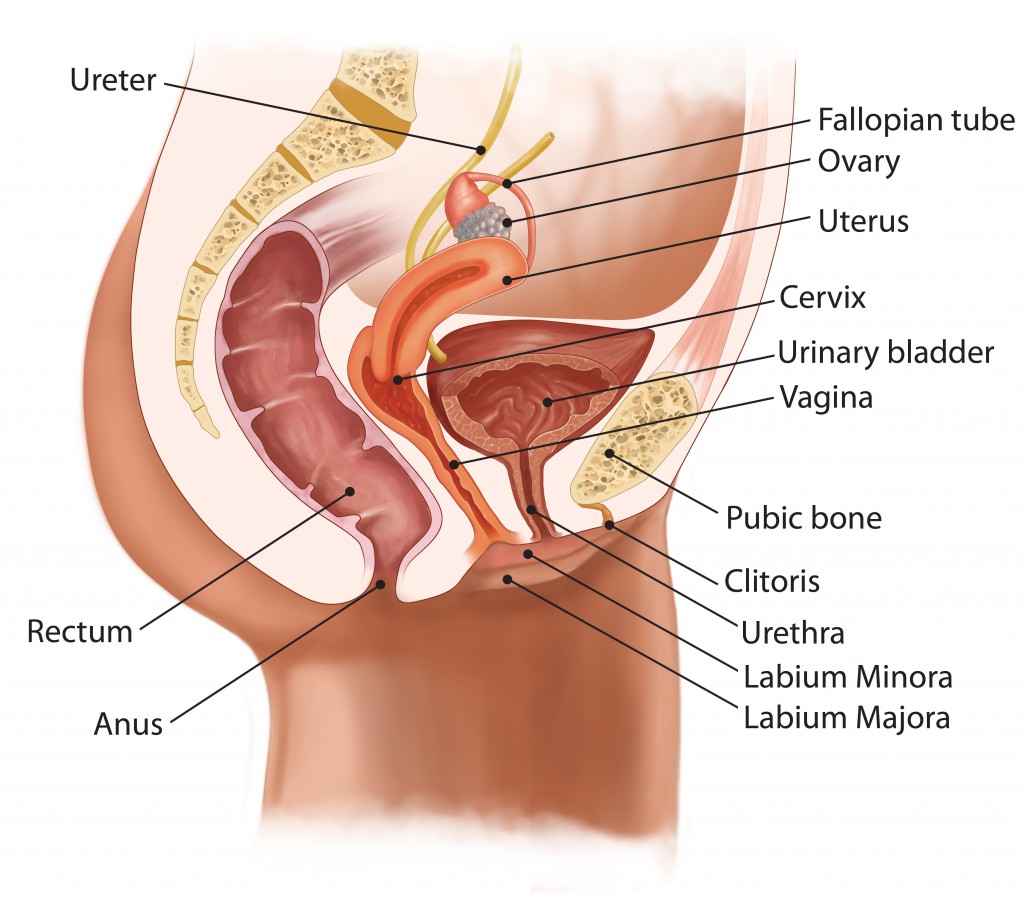
It may take weeks and even months after infection before any symptoms of genital warts appear because the virus can lie undetected in the body for a very long time. The warts may appear as a single wart or multiple warts and can be small or large in circumference. They can also be located in a central region or located in various locations in the genital area including the anus and thighs. One complication of genital warts could be an extensive outbreak which has been known, in rare cases, to obstruct the urethra, vagina or anus. In these types of cases, surgery is often necessary, but again, these cases are rare.
Causes
The cause of genital warts is from the human papillomavirus that lives on the skin of every person. Certain types of this virus cause genital warts why other types are also known to be the cause of common warts on the body, and though of a different type, they can also be transmitted through skin-to-skin contact.
The human papillomavirus lives in and on the body undetected and most carriers are not aware that they have the virus that is spread sexually. Of the 100 know types of the virus, only a small portion cause complications. These are the high risk and low risk types of the virus. 90% of genital warts are caused by the two low risk types of HPV, type -6 and -11. The high risk types are HPV -16, -18, -31 and -45 which are known to give rise to cancer.
Risk Factors
Genital Warts are highly contagious and can be transmitted through first time intimate encounters or sexual contact. Not having sex is the only way to reduce the potential for infection of the type of HPV that cause genital warts. Because the disease is primarily transmitted through skin to skin contact, wearing a condom will not always prevent transmission.
A person may not know they are carrying the disease because they are not exhibiting any of the symptoms of an infection, and regardless of protection it is an almost certainty that they will spread the virus. Both women and men generally do not exhibit symptoms of HPV unless they have the visible genital warts and sometimes, the warts are not visible.
Someone can still be a carrier of the disease and they can readily transmit it to their partners unknowingly. HPV and genital warts is often known as a silent virus as well as a silent sexually transmitted disease because of the potential to never exhibit symptoms.
Prevention Tips
The only sure prevention against contracting genital warts and HPV is by not having sex. Because the virus lives on the skin, anytime uninfected skin comes into contact with an infected person, the risk of contracting genital warts and HPV is real. Therefore, wearing condoms cannot prevent the spread of genital warts or HPV unless the warts are completely covered. Because genital warts are highly contagious, just touching genital areas can also spread the disease if a person does not wash afterward.

Having multiple sex partners can also increase your risk of contracting genital warts and HPV. Another risk increase is having a partner who has previously had multiple partners. It is best to understand your partner’s history before engaging in sex, though this is no indication that they do not already carry the virus, and use of protection could potentially lower your risk but is not a guarantee with genital warts and HPV.
Touching the warts and then touching healthy skin can result in an infection over half of the time. If you think you may have genital warts, seek the advice of your doctor and maintain clean hygiene practices to prevent the spread of the warts on your body.
Once contracted, the spread of genital warts is not preventable unless the carrier stops having sex altogether. Condom use can lower the risk, but not completely eliminate it. However, the drug Gardasil was approved in 2006 for the prevention certain HPV types including those that cause genital warts. The drug has not been tested for its effectiveness in curing genital warts, but is effective in prevention. It has been approved for girls and women aged 9 to 26. It is being tested for effectiveness in older women and in men.
Tests and Diagnosis Considerations
Genital wart tests and exams are primarily visual exams given by a health care professional. To verify if the symptoms are indeed caused by genital warts, a doctor may use a 5% acetic acid to turn the potential infected area white. However, the acid may also turn healthy skin white, thus it is difficult to determine from the acetic acid alone.
Because there are no tests specifically designed to test men to determine if they have HPV, unless they exhibit symptoms of genital warts, they will not know they carry the disease. The only test for HPV is for women who have been requested to do a follow up procedure for a pap smear with abnormal results. This test will determine what type of HPV the woman has and whether or not she has the high risk HPV, forms associated with cervical cancer. In addition, the woman can exhibit the symptoms but carry a low risk HPV that will not threaten her cervical safety.
Often times, receiving an abnormal Pap smear result is how a couple will discover that one of the partners has HPV. If the woman has HPV, it can safely be assumed the man will have HPV whether or not he exhibits the symptom of genital warts. Because HPV can live in the body for years without detection, the sudden rise of genital warts does not necessarily mean that a partner has been unfaithful. It may have just taken a while for the virus to show up on the outside of the genital region or internally through an abnormal pap smear. Again, the genital warts may not actually be visible and can be present for years without the person’s knowledge.
Treatment Options
Genital warts can be treated in a variety of ways which may or may not be successful. The virus still has the potential to come out as genital warts years, months and even weeks after treatment. There are many treatment options should one or the other not work.
Topical Treatments
Topical treatments include many options including treatments applied by a health care professional or applied at home by the infected person. These topical treatments can have good success as long as the treatment is applied as directed and for the length of time specified. Other treatments include medical procedures that need to be administered by a health care professional. These treatments include:
Cryotherapy
Cryotherapy is the freezing of the genital warts by a health care professional. This treatment can be painful but has no other side effects usually and is lower in cost than the other options such as laser and electrodessication.
Laser Treatment
Laser Treatment is the next level of treatment that can be used by a healthcare professional to burn, or cut, the warts off of the infected area. This is a more expensive option and can have detrimental side effects including scarring of the infected areas.
Electrodessication
Electrodessication utilizes an electrical current to destroy the warts and can be painful as well as ineffective in completely removing them all. Electrodessication is expensive and is not commonly suggested as a treatment option. When visiting your health care provider for genital warts, be sure to discuss all your options if the initial treatment does not work.
Surgeries
Surgery is sometimes used when there has been no response to any of the previously mentioned treatments or when the warts are small in size and in number. It may also be necessary if the warts are blocking the urethra, vagina or anus.
Home Remedies
There are no known home remedies or herbal treatments that are effective at treating genital warts. While medical treatment can be effective in reducing the symptoms of the low risk HPV infection known as genital warts, treatment does not mean the carrier is cured. They will carry virus the rest of their lives, whether or not the virus is dormant will not be known and possible infection to another sexual partner is always a possibility.