Sore Nipples
Causes, Prevention and Remedies
Though it might seem like an embarrassing problem, many people experience sore nipples from time to time. Sore nipples don’t necessarily indicate that anything is wrong, and thus the issue usually isn’t really considered a medical condition. However, though typically benign, there are some cases in which sore nipples could indicate more serious, underlying medical conditions.
There are several common causes for breast pain of all types, including nipple tenderness; luckily, there are also many soothing remedies for treating sore nipples. Here, those concerned about sore nipples and other types of breast pain can explore different reasons why a person might experience this painful and sometimes embarrassing problem, and what options exist for treating it.
Common Causes of Tender or Sore Nipples
Breastfeeding mothers are likely the group most heavily affected by nipple pain or other types of breast tenderness. Of course, there is the potential the soreness is simply a result of increased hormone levels, but in the case of women who breastfeed their children, there are also many other factors at play.

The very process of lactation, or milk production, increases a woman’s chances of developing an infection of the milk ducts called mastitis. Mastitis is a condition that can result in not just sore nipples, but incredibly painful breasts. If a milk duct becomes clogged, and bacteria begins to breed, a woman may develop fever, hardening of the breasts, and excruciating pain. The often jolting, almost electric pains will sometimes radiate through the affected breast and come in unpredictable waves, often feeling as if they are coming straight through the center of the nipple.
Hormones
In women who are not pregnant, hormones may play the biggest role in sore nipples and breasts. In menstruating women, levels of certain hormones elevate dramatically in the week or so before their periods, especially a hormone called progesterone. Progesterone is the hormone responsible for holding on to things to nourish a baby in the womb, should one be conceived during a given cycle. This retention includes water retention, and this process is carried out heavily in the breasts.
The heavy, full feeling of a woman’s breasts and sore nipples suffered prior to menstruation are often described as bothersome and painful, and not unlike what women in the very early stages of pregnancy experience. However, if a woman is pregnant, she will likely not menstruate and so the heavy, sore feeling will not fade for weeks until hormone levels balance out for a time. Later in pregnancy, the breasts may become painful again due to fluctuating hormone levels and eventually, lactation.
New Mothers & Sore Nipples
Nipple pain, chapped nipples and tenderness of the breasts is extremely common in new mothers who breastfeed, even when no mastitis is present. The painful side effects of breastfeeding can often be caused by the very act of nursing itself. The strong suction the baby’s mouth creates during nursing is necessary for encouraging milk flow and stimulating the “let down” of mother’s milk, but it can sometimes chafe and chap the delicate skin of the mother’s nipple. This can result in painful continued nursing, the stress and pain of which can actually inhibit milk production.
Breastfeeding Concerns
Some women who experience pain while breastfeeding give up and switch to formula far earlier than they intended to. In this way, sore nipples can actually affect the health of the baby and the emotional well-being of the mother. Many nursing mothers feel as if they have failed their child when they decide to stop breastfeeding, and this can lead to an increased risk of the mother developing post-partum issues, including post-partum depression and anxiety. If the nipple or breast pain is so severe that a woman is considering giving up nursing altogether, she should seek the professional guidance and assistance of a certified lactation consultant before deciding to stop.
Women who do decide to stop nursing may initially experience increased pain and sensitivity of the breasts, nipples and areola as the milk supply will continue to build in anticipation of the baby’s needs. If a week or two passes with no nursing and no release of milk, the body’s natural signals to produce more milk will begin to dissipate, and the swollen, tender glands and tissues will eventually respond. Expect full relief from breast and nipple soreness after two weeks of quitting breastfeeding.
Menopause
Menopausal women who experience sore nipples or breast tenderness may be suffering from severe hormone fluctuations, and will often experience other symptoms as well. Other symptoms that may indicate a hormonal imbalance related to menopause include missed or irregular period with no chance of pregnancy, mood swings, fatigue, hot flashes and irritability.
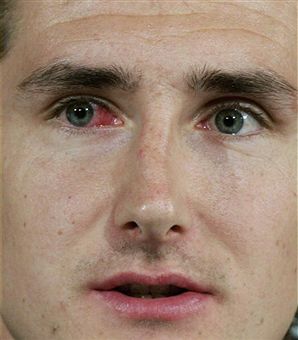
For women who don’t fit in the above categories, and for men who are experiencing sore nipples, it is possible there may exist a skin condition which is affecting the nipples and causing discomfort. Rashes from personal products, dermatological issues or clothing that irritates the skin and rubs across the nipples may cause pain. This type of condition is usually easily reversed by applying a bit of petroleum jelly and wearing loose, soft clothing over the area until healed.
Gynecomastia
Less common than nipple tenderness in women, men may experience sore nipples if they have a condition called gynecomastia. Gynecomastia is a term that describes when breast tissue grows abnormally on a male chest, usually undesired by the patient. This condition can include pain and swelling of the breast tissue, including the nipple.
Finally, in both men and women, sore nipples and other types of breast pain can have serious medical implications if there are also other risk factors for breast cancer present. Lumps in the breast tissue, nipple discharge or bleeding from the nipple and other warning signs may dictate a visit to a medical professional skilled in breast health to determine what these symptoms mean. In cases of nipple and breast pain where breast cancer is a concern, further testing in the form of lumpectomy, biopsy and blood tests may be necessary to rule out the possibility of cancer.
Prevention of Sore Nipples and Painful Breasts
In women, the group most commonly afflicted by this problem, wearing a bra that fits correctly may be the first step in preventing pain. Bras that fit incorrectly may place undue or unbalanced strain on the breasts, causing inflammation and pain.
Reducing friction against clothing can also help relieve nipple soreness. Choosing soft, cotton bras and shirts can significantly help in this arena. Synthetic materials may aggravate sensitive tissues of the areola and nipple, as can ingredients in some body care products. Evaluating environment and lifestyle habits can produce good results from recurring sore nipples.
Since progesterone involves holding onto what is put into the body, and estrogen can increase swelling of breast tissue and glands, limiting the intake of caffeine and other stimulants can help reduce the hormonal impact. Staying well-hydrated and avoiding things that cause the body to naturally hold onto water and bloat, such as salt and caffeine, can considerably affect swelling and pain of the nipples and breasts.
Medical Treatment and Home Remedies for Sore Nipples
In the case of breastfeeding mothers, sore nipples can sometimes be helped with various over-the-counter creams and salves. These creams are specially designed for lactating mothers and can help sooth and protect the delicate and easily-chafed skin of the areola and nipple. These nipple creams are widely available and relatively inexpensive. Nursing creams and nipple salves can be found in many retail stores, especially those geared toward baby care and new mothers.
For breastfeeding women, one avenue to relief from breast and nipple pain may be through an appointment with the lactation consultant at the hospital where they delivered. Incorrect latching of the baby can cause increased nipple chafing and pain, and sometimes all that is required to correct the problem is to correct baby’s positioning during nursing. Learning proper “latch-on” and “latch-off” techniques can help new mothers continue to breastfeed with less pain, which is beneficial to both mother and child.
Lactation Consultants
Certified lactation consultants may be able to recommend a certain cream over another, but recommendations from other mothers can be just as valuable. Petroleum jelly may be used for some cases, but is not generally recommended as highly as creams specifically designed for use by nursing mothers, as the petroleum can block the openings in the nipples and inhibit milk flow. This can cause a blockage in the milk ducts, and can exacerbate the soreness. For those who are not lactating but who are experiencing raw or chapped nipples and areolas, the use of petroleum jelly is perfectly safe.
Home Remedies
A warm shower is an easy home remedy for sore nipples and tender breasts, especially in pregnant or lactating women. However, depending on the severity of the pain, some women may not be able to tolerate the water stream beating down on the swollen and painful breast tissues. In these cases, a warm washcloth applied to the affected breast can help soothe and relieve pain in a more controlled and comfortable manner.
For anyone who is suffering sore or chafed nipples, steeping chamomile tea bags in hot water and then applying the tea bags to the nipple or other sore areas of the breast can help relieve swelling. When using this home remedy for sore nipples, it is imperative to test the warmed tea bags on the wrist or back of the hand before applying to the breasts to avoid burning the sensitive skin on the nipple. Excess water should be squeezed from the tea bags before application, but they should not be well wrung-out as the heat trapped in the moisture is what will help provide relief.
Nipple Shields
Nipple shields are another good option for nursing mothers who are experiencing nipple and areola pain. Various versions of this product are widely available at baby care retailers and drug stores. Nipple shields help protect nipples by reducing friction against clothes and preventing further irritation to the delicate membranes. Nipple shields are usually made of soft fabric, and are designed to adhere to the inner cups of a woman’s bra to prevent shifting. They are an inexpensive and effective tool for new mothers to help provide relief between feedings.
Hormone Replacement Drugs
In men or women for whom a hormonal imbalance has resulted in troublesome nipple or breast pain, oral hormone replacement drugs or medicated creams that help deliver hormones topically may be indicated. Only a physician can make this determination, and will do so through a series of tests and screenings.
For any severe pain of either the nipple, areola or other breast tissue, or in cases where any discharge besides milk is seen coming from the nipple, a doctor’s evaluation is the best course of action for quick relief and to rule out any serious underlying medical conditions. Over-the-counter medications such as acetaminophen or ibuprofen may help provide relief, but a doctor can prescribe stronger narcotic pain killers which may allow a woman to safely continue to breastfeed without pain. The risks-to-baby and benefits-to-mother ratio will be weighed before the decision to prescribe heavier medications is made.