Dry, Peeling Skin: Causes, Prevention Tips and Cures
Peeling skin is a fairly common medical affliction that affects millions of people every year, and some are faced with the issue on a long-term basis. Skin may peel or dry skin can occur for a number of reasons and vary greatly in the level of severity. Besides being an annoying and often embarrassing problem, peeling skin can sometimes indicate that serious damage has occurred to the top layers of skin. In more rare cases, it can also indicate serious underlying medical conditions.
The following text is presented for educational and informational purposes only, and is no substitute for a diagnosis by a medical professional. If you are concerned about your skin or are experiencing troubling symptoms, see your doctor.
Here, explore some of the most common causes for peeling skin, and find out ways to both prevent and treat this condition. If the manifestation of skin problems turns out to be just one symptom of a more serious underlying condition, treatment for the related problem will likely help clear up any peeling.

Common Causes of Dry and Peeling Skin
Skin may begin to peel in relation to extreme dryness. In many instances of extreme skin dryness with peeling, sun exposure can be determined to be the main culprit. Sun exposure can cause skin irritation or damage even when sunblock is used.
This lapse in protection can occur when the exposure time is excessive, if the SPF value of the sunblock is less than 30, if the sunblock is not reapplied regularly or in rare cases where a person cannot tolerate any direct sunlight at all.
Sunburn & Heat Exposure
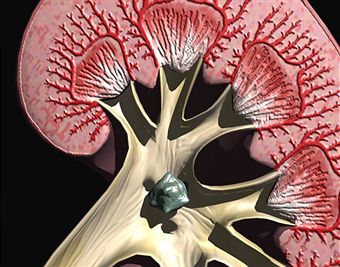
Sunburn is a major cause of sun-related peeling skin. After the initial injury to the top layer of skin cells from intense direct sunlight, the skin cells dry up, die and will eventually peel or slough off. Raw, painful skin may be revealed under the peeling skin if the damage extended beyond the very first layer, also called the epidermis. The “shedding” of old, damaged skin cells from the epidermis is a natural process when the skin is damaged, and may actually be a natural defense mechanism. To protect the body from damaged cells and allow new cells to generate, the old skin must die and fall away.
Heat exposure without sun is another common cause of peeling skin, increased dryness and other skin irritations. Sun and heat exposure can make skin appear red, itchy and feel hot long after the exposure occurs. Skin may blister in response to a severe sunburn or heat burn, and these types of burns should be evaluated by a doctor. After a period of blistering, usually two to five days, the deadened skin will peel away or “shed”.
Chronic Conditions & Chemicals
Certain chronic skin conditions, such as eczemas or types of dermatitis, can also result in peeling skin. Even babies can display scaly, flaking or peeling skin; this affliction is commonly referred to as “cradle cap”, and it is a type of childhood eczema. The condition has a medical name of seborrhoeic dermatitis, which is just a fancy way to describe yellowed, scaly skin that flakes off of an infant’s head. See possible treatments below.
Chemical exposure can also cause dry skin, and this is most evident on the hands of those who work with them on a regular basis. Even frequent hand washing or use of hand sanitizers, which are deemed necessary by most to prevent the spread of germs, are incredibly damaging to skin. This is especially true in people with sensitive skin. Seeking out soap and other products that won’t dry out the hands is a smart solution for those who must wash up more than five to ten times a day on a regular basis.
Fungi
Certain fungi, such as athlete’s foot, ringworm and jock itch, can also cause skin to slough or peel off. Staph infection and eczema also commonly result in the patient experiencing reddened, itchy, peeling or sloughing skin. These conditions should be treated by a doctor with an anti-fungal or antibiotic regimen to clear up the problem. They are unlikely to go away on their own and can turn serious if left untreated.
In many cases where skin irritation occurs without obvious cause, such as fungi, sunburn or other underlying medical conditions, a bit of peeling skin or dry patches may indicate nothing more than a need for a few lifestyle changes. Poor diet, inadequate water consumption, smoking, vitamin deficiencies, excessive alcohol intake, and, ironically, too much exposure to water can all lead to dry skin and other skin problems.
Serious Conditions
Sometimes, though, peeling skin and extreme dryness may be indicative of a much more serious medical condition. Some types of lymphoma and skin cancer will present with a list of symptoms that includes peeling skin, though only a doctor or other trained medical professional can make that determination.
In some rare diseases, such as with Kawasaki disease and peeling skin syndrome, dry skin and peeling can be a typical symptom. These diseases need to be treated and closely monitored by a medical professional.
Solutions For and Prevention of Dry and Peeling Skin
If a serious underlying medical cause can be ruled out, and peeling skin is just a bothersome, nuisance problem, it is likely a condition that can be treated at home. There are many simple ways to help heal damaged skin and actually begin to replenish moisture in skin at home.
Dry skin may be a result of simple dehydration. Getting started on an active regimen of six eight-ounce glasses of water daily for at least two weeks may markedly improve the feel and appearance of the skin. This is an easy and inexpensive way to try and solve problems with dry skin without a trip to the dermatologist.
Maintaining proper hydration is keenly important to the function of all organs of the body, and the skin is the largest organ of all. Furthermore, the skin is the only organ worn on the outside of the body, exposed to all sorts of external toxins and irritants on a regular basis. Air conditioning or incredibly hot weather outdoors in the summer months can cause dry skin, as can turning on the heater in the winter.
Using Moisturizers
Using a good moisturizer will dramatically improve conditions if the skin is already dry and damaged, and help prevent the problem from recurring. For those with sensitive skin, checking the labels of new body products for known irritants in the ingredients list can help them avoid making the problem worse. There are creams and lotions which have collagen and silicone as main ingredients, and these may help improve the condition of dry, chapped, peeling skin on the hands especially.
The Effects of Water
Cold water can help tighten pores and promote healing of skin cells, so turning the water to ‘cool’ toward the end of a shower may help with peeling and dried out skin. blotting skin after showering or swimming, as opposed to rubbing vigorously can help protect skin. Even a bit of olive oil rubbed into the skin once a week can help replenish skin tone, feel and texture, and may reduce itching, peeling and dryness.
Avoid excessively hot water, as well. While an occasional dip in a heated pool or hot tub is fine, taking scalding hot showers every day is not a good idea. Especially in areas with very dry weather, exposure to water of any kind on a daily basis may promote dry skin and peeling. Showering only every other day during a flare-up of dry or itchy skin and limiting the use of body products that may worsen the problem can help the skin’s moisture levels from being stripped each day.
Washing Daily & Oils
Skin produces natural oils, and these oils serve as a protectant as well as a conditioner. For those with overly greasy complexions, these oils may seem like the enemy. For someone with impossibly dry skin, however, the word “oil” is one of the nicest words in the English language. While many people may shudder at the thought of not washing up every single day, our skin wants a break now and then. Not showering doesn’t mean not washing parts that warrant daily washing, and it doesn’t mean not putting on fresh clothes. Especially with the advances of deodorants and perfumes, most people simply do not truly need a daily shower.
Contact a Dermatologist
If the dry skin and peeling is too painful or severe to treat at home, a dermatologist or a family doctor may be able to provide some other options. Some cases of dry, cracking skin are so resistant to less aggressive treatment that powerful steroid-infused ointments and lotions must be used, usually with some good measure of success. Pain medications can also be prescribed to help the patient handle the discomfort of a severe sunburn, chemical burn or heat related burn.
Home Remedies & Creams
At home, those suffering painful sunburns can take over-the-counter anti-inflammatory drugs such as naproxen and acetaminophen, and apply a topical aloe vera gel to the affected areas. Do not apply salves to blistered skin without a doctor’s recommendation.

Medicated steroidal creams, called corticosteroids, can help babies suffering from cradle cap and other types of dermatitis. While these creams have been shown to be effective, many doctors simply recommend washing the hair with baby shampoo and scrubbing the scalp gently with a washcloth every other day. Many doctors and mothers also recommend massaging baby oil into the scalp after washing baby’s hair. Out of baby oil? Try a few drops of olive oil from the pantry or mineral oil from the medicine chest instead.
Though some people may also claim petroleum jelly will help cure dermatitis of the scalp, the greasiness can actually contribute to the problem. If the condition appears to make the child fussy due to itchy or painful eczema, petroleum jelly will provide soothing relief. In cases where the scaly, yellow patches of crusty skin extend beyond the scalp or behind the ears, such as when they may appear on the child’s face, bother the child excessively, or if the condition has been getting worse over time, it is prudent to see a doctor.
When To Worry About Skin Conditions
Whenever skin is burned so badly that it blisters, if there is an unexplained rash that persists for more than a few days or gets worse, when unusual, new growths are noted or when severe pain accompanies any of the aforementioned, it is time to seek immediate medical attention from a qualified professional.
When possible, go to a skin doctor, or dermatologist, for any serious skin concerns, as this is their primary area of expertise. After all, a person wouldn’t go to a foot doctor for a tooth ache. Most general family practitioners are qualified to handle skin conditions, and you may need to visit one initially to satisfy the referral requirements to see a specialist under your medical insurance, but a dermatologist will likely be more up-to-date in the skin care field and in their knowledge of available treatment options.
A dermatologist will also likely be able to diagnose the root cause of any peeling skin from the onset, and this will help promote speedy but accurate treatment. If skin cancer is determined to be the cause of the symptoms, a skilled dermatologist will likely be able to immediately coordinate a treatment plan, and may refer the patient to an oncologist who specializes in the treatment of that particular cancer, if necessary.